CASE REPORT

Foveal Findings As A Sign of Familial Adenomatous Polyposis: A Case Series and Review
PRESENTING AUTHOR
Davina A. Malek
-
Serena Shah,Department of Ophthalmology, Bascom Palmer Eye Institute, University of Miami Miller School of Medicine. 900 NW 17 Street. Miami, FL 33136.
-
Francisco Lopez-Font,Department of Ophthalmology, Bascom Palmer Eye Institute, University of Miami Miller School of Medicine. 900 NW 17 Street. Miami, FL 33136.
-
Jason Fan,Department of Ophthalmology, Bascom Palmer Eye Institute, University of Miami Miller School of Medicine. 900 NW 17 Street. Miami, FL 33136.
-
Natasha Ferreira Santos da Cruz,Department of Ophthalmology, Bascom Palmer Eye Institute, University of Miami Miller School of Medicine. 900 NW 17 Street. Miami, FL 33136.
-
Audina M. Berrocal,Department of Ophthalmology, Bascom Palmer Eye Institute, University of Miami Miller School of Medicine. 900 NW 17 Street. Miami, FL 33136.
-
Purpose:
To report 2 cases of presumed retinal astrocytic hamartoma (RAH) in pediatric patients with genetically confirmed familial adenomatous polyposis (FAP), both evaluated by optical coherence tomography (OCT) and one assessed with optical coherence tomography angiography (OCTA).
-
Case Report:
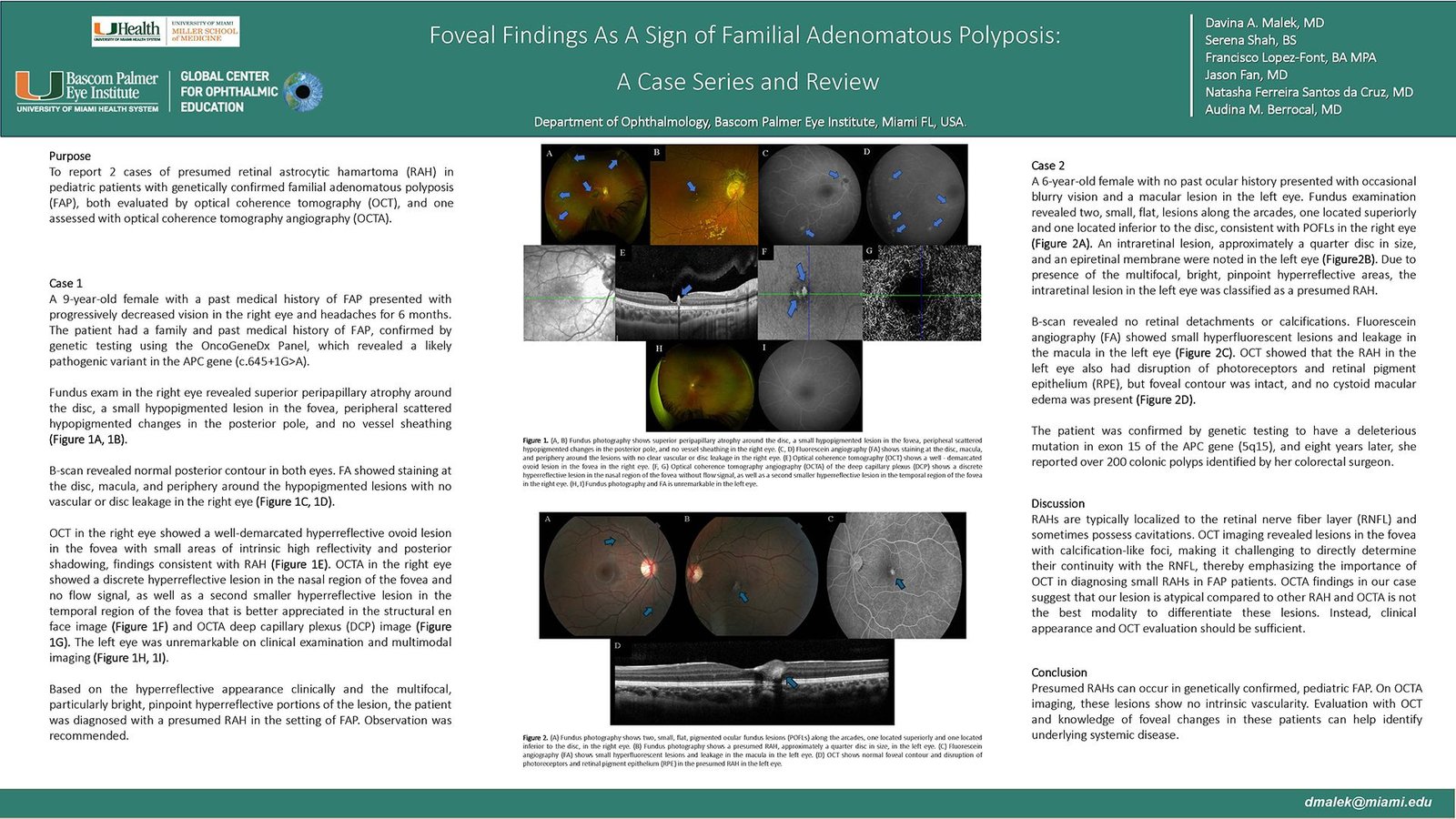
A six-year-old girl presented with occasional blurry vision in the left eye. OCT showed a foveal hyperreflective lesion with photoreceptors and retinal pigment epithelium (RPE) disruption. A nine-year-old female with a past medical history of FAP presented with progressively decreasing vision and floaters in the right eye for the past 6 months. OCT showed a well-demarcated hyperreflective ovoid lesion in the fovea. OCTA revealed no flow signal within the lesion, as well as a second smaller hyperreflective lesion temporal to the fovea. Both patients were diagnosed with presumed RAH in the setting of FAP.
-
Discussion:
RAHs are typically localized to the retinal nerve fiber layer (RNFL) and sometimes possess cavitations. OCT imaging revealed lesions in the fovea with calcification-like foci, making it challenging to directly determine their continuity with the RNFL, thereby emphasizing the importance of OCT in diagnosing small RAHs in FAP patients. OCTA findings in our case suggest that our lesion is atypical compared to other RAH and OCTA is not the best modality to differentiate these lesions. Instead, clinical appearance and OCT evaluation should be sufficient.
-
Conclusions:
Presumed RAHs can occur in genetically confirmed, pediatric FAP. On OCTA imaging, these lesions show no intrinsic vascularity. Evaluation with OCT and knowledge of foveal changes in these patients can help identify underlying systemic disease.
The authors have no financial interests in any material discussed in this article. There are no conflicts of interest to disclose.